The symptoms and the disease is usually progressive and worsens with increasing hypoestrogenism and makes life miserable for some by decreasing the quality of life in those senile years.
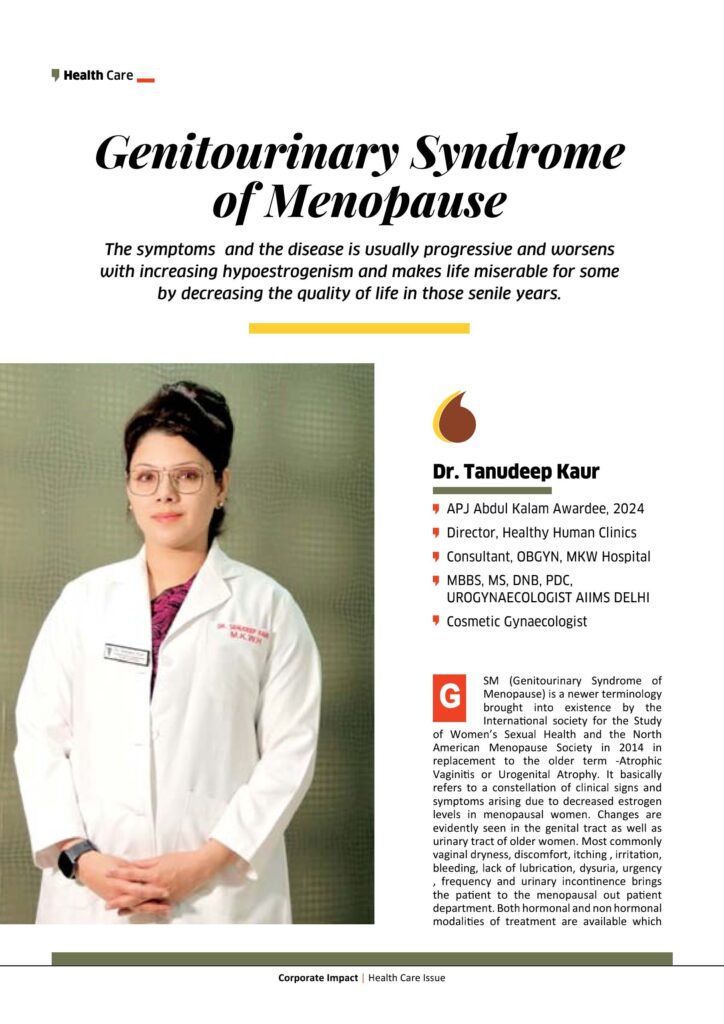
Dr. Tanudeep Kaur
APJ Abdul Kalam Awardee, 2024
Director, Healthy Human Clinics
Consultant, OBGYN, MKW Hospital
MBBS, MS, DNB, PDC, UROGYNAECOLOGIST AIIMS DELHI
Cosmetic Gynaecologist
GSM (Genitourinary Syndrome of Menopause) is a newer terminology brought into existence by the International society for the Study of Women’s Sexual Health and the North American Menopause Society in 2014 in replacement to the older term -Atrophic Vaginitis or Urogenital Atrophy. It basically refers to a constellation of clinical signs and symptoms arising due to decreased estrogen levels in menopausal women. Changes are evidently seen in the genital tract as well as urinary tract of older women. Most commonly vaginal dryness, discomfort, itching , irritation, bleeding, lack of lubrication, dysuria, urgency , frequency and urinary incontinence brings the patient to the menopausal out patient department. Both hormonal and non hormonal modalities of treatment are available which provide relief and help in improving quality of life scores in these women.

70% of GSM patients do not come to the doctor due to shyness , embarrassment and because they take it as a normal part of their aging process. The symptoms and the disease is usually progressive and worsens with increasing hypoestrogenism and makes life miserable for some by decreasing the quality of life in those senile years. The commonly reported symptoms are;(8,9).
Pathophysiology
The basic interplay is of severely decreased estrogen levels along with evidence of plummeting androgen levels which may cause loss of structural and functional integrity of the genitourinary tissues justifying supplementing androgens in the treatment of libido and dyspareunia in these women.
Estrogen present predominantly circulating in premenopausal patients maintains the collagen content leading to its increased thickness and elasticity and the moistness of the epithelium along with the optimal blood supply. A healthy vaginal microbiota with an acidic ph ranging between 3.5-5 and protection from vaginal infections and recurrent UTI is also a feature of the premenopausal estrogen levels. On the contrary a decline in estrogen levels by 95% to around 5pg/ml in postmenopausal women from around 50 pg/ml is responsible for the various atrophic menopausal changes.

Increase in vaginal ph to >/= 5 in menopausal age group due to decreased glycogen content leads to overgrowth of recurrent and resistant infections.
Loss of elasticity of vaginal and urinary tissues leads to shortening and narrowing of vagina and prolapsing of urethra forming a urethral caruncle. Also, the decreased frequency of coitus in this age group is an important cause of the above atrophic changes as compared to a premenopausal vagina with regular sexual intercourse activity. Reduction of vaginal secretions from 3-4 gm/4 hours to 1.7 gm/4 hours leading to vaginal dryness.
Thinning of the superficial epithelial cell layers to even their absence with increasing age and loss of rugae and increase in subepithelial connective tissue leads to increased susceptibility of vaginal and urinary epithelium to bleeding, trauma, ulceration with pressure, petechiae and pain during sexual intercourse. Also, Recurrent urinary infections along with overactive bladder symptoms, frequency, urgency, dysuria, heamaturia and pelvic organ prolapse is common.
Some common symptoms being;
• Decreased vaginal lubrication during sex which usually maybe the first presenting sign during the perimenopausal period.
• Dyspareunia at the introital entry or inside the vagina.
• Postcoital bleeding or labial fissures or unexplained vaginal or vulval bleeding.
• Hypoactive sexual desire with decreased arousal or lack of orgasm.
• Unexplained Vulvovaginal irritation , itching or burning.
• Vaginal discharge which may be leucorrhoea or yellowish & malodorous discharge.
• Leveator spasm – Tense leveator muscles, ie increasing muscle tension on touching the posterior vagina.
• Urinary symptoms and Urethral discomfort due to urethral caruncle or prolapse.
Initial line of therapy – Nonhormonal vaginal lubricants and moisturizers.
Vaginal moisturizers- use 2-3 days/week and also during sexual activity as they are typically bioadhesives. The main ingredient being hyalouronic acid.
Lubricants are mainly used only during the sexual act and are usually water based or can be oil based or silicone based.
Second line of therapy- Vaginal estrogen therapy is very effective in decreasing vaginal dryness and discomfort, in ameliorating urinary symptoms ,and vaginal and urinary infections and almost all severe symptoms of vaginal atrophy because it restores normal vaginal microflora, improves vaginal ph, thickens the epithelium and hence prevents dyspareunia.
GSM is a treatable condition and requires regular consultation with a gynecologist and in particular a urogynecologist.